Regional & Topical Anesthesia for Endotracheal Intubation
Recent developments in regional anesthesia have resulted in a number of innovative and refined options to practitioners, often allowing regional techniques to be used for patients with presumed difficult airways. However, not every surgery can be performed under regional anesthesia. In addition, even in the hands of the most skilled regional anesthesiologist, blocks are subject to a certain rate of complications or failure.1−4 In addition, there are many situations in which the anesthesiologist is called on to secure an airway in less than ideal circumstances. Expertise with regional anesthesia of the airway allows intubation in awake patients with suspected difficult intubation, upper airway trauma, or cervical spine fractures. Therefore, it is essential that every regional anesthesiologist be skilled in the administration of general anesthesia and especially in the management of the difficult airway.
In recent years, there have been many advances in difficult airway management. The introduction of the laryngeal mask airway, and later the intubating laryngeal mask airway have changed the American Society of Anesthesiologists’ difficult airway algorithm significantly.5 Despite new devices and techniques being added to the arsenal daily, the mainstay of difficult airway management remains flexible fiberoptic laryngobronchoscopic intubation. Fiberoptic intubation can be performed under a variety of conditions. However, one major decision must be made with every procedure will the patient be intubated while under general anesthesia, or does the patient need to be awake during intubation?6 Intubation under general anesthesia (even with inhalational induction and spontaneous respiration) carries the inherent risk of losing control of the difficult airway. For this reason, many anesthesiologists, on recognition of a difficult airway, elect to perform an awake intubation using either fiber optic laryngobronchoscopy or awake direct laryngoscopy.
Direct laryngoscopy in an awake, unprepared patient can be extremely challenging. Excessive salivation and gag and cough reflexes can make intubation difficult, if not impossible, under awake conditions. In addition, the stress and discomfort may lead to undesirable elevations in the patient’s sympathetic and parasympathetic outflow. Several highly effective topical and regional anesthesia techniques have been developed to subdue these reflexes and facilitate intubation. Each of these techniques has the common goal of reducing sensation over the specific regions that will be encountered by the fiber optic bronchoscope and endotracheal tube.
Relevant Anatomy
To decide on a proper approach to an awake fiberoptic intubation, one must determine what structures need to be anesthetized along the two basic routes of intubation (oral or nasal) to facilitate optimal surgical conditions in the context of patient-specific anatomic considerations. Each of these routes has a well-defined pattern of innervation that can be specifically blocked to provide adequate anesthesia.
The nasal cavity is innervated by the greater and lesser palatine nerves and the anterior ethmoidal nerve. The palatine nerves arise from the pterygopalatine ganglion and innervate the nasal turbinates and most of the nasal septum. The pterygopalatine ganglion is located posterior to the middle turbinate in the pterygopalatine fossa. The anterior ethmoidal nerve arises from the olfactory nerve (CN I) and innervates the nares and the anterior third of the nasal septum.7
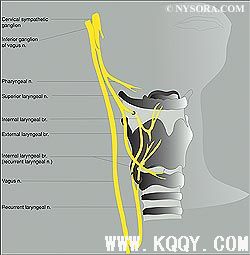
The oropharynx is innervated by branches of the vagus, facial and glossopharyngeal nerves (Figure 1). These nerves travel anterior along the lateral surface of the pharynx, and the three branches provide sensory innervation to the posterior third of the tongue,[8] the vallecula, the anterior surface of the epiglottis (lingual branch), the walls of the pharynx (pharyngeal branch), and the tonsils (tonsillar branch). The sensory innervation of the anterior two thirds of the tongue is provided by the trigeminal nerve (lingual branch of the mandibular division).8 Given that it is not a part of the reflex arcs controlling gag or cough, its blockade is not essential for comfort during fiberoptic intubation.
The internal branch of the superior laryngeal nerve is a branch of CN X (vagus nerve) (Figure 2). The superior laryngeal nerve provides sensory innervation to the base of the tongue, posterior epiglottis, aryepiglottic folds, and arytenoids.7 This branch originates from the superior laryngeal nerve lateral to the greater cornu of the hyoid bone. The recurrent laryngeal nerve provides sensory innervation of the vocal folds and trachea and motor function of all intrinsic laryngeal muscles except the cricothyroid supplied by the external branch of the superior laryngeal nerve.7
| Clinical Pearls | |
|
|
Techniques for Anesthetizing the Airway
Preparation for Awake Intubation
The process of intubating an awake patient requires careful preparation. The anesthesiologist must evaluate each patient’s needs on an individual basis. Nearly every patient experiences some degree of anxiety associated with the surgery, anesthesia, and perhaps outcome. For this reason, most patients require some degree of sedation and analgesia. For this purpose, it is best to use short-acting or reversible agents for sedation or agents that do not cause a considerable degree of respiratory depression. Some examples of commonly used medication for awake intubation include midazolam, alfentanil, and fentanyl. These sedatives/analgesics are particularly useful in this setting because of their easy titratability to effect easy reversal with flumazenil or naloxone. Similarly, dexmedetomidine does not cause respiratory depression and is suitable in this setting.9
Antisialogogues should be used before any airway instrumentation. Oral secretions may make visualization via the fiberoptic equipment difficult and may serve as a barrier to effective penetration of local anesthetic into the mucosa. Glycopyrrolate 0.4 mg given intramuscularly or intravenously helps to diminish secretions.10 Alternatively, atropine 0.5–1 mg may be used intramuscularly or intravenously to similar effect. Intramuscular administration is favored over intravenous administration to avoid undesired side effects such as tachycardia and, less commonly, psychosis (with atropine) (Table 1).
| Table 1: Commonly Used Medications and DosagesWith Their Reversal Agents | |||
| Medication | Dosage and Route | Effect | Reversal Agent |
| Atropine | 0.5–1 mg IV, IM | Antisialogogue | N/A |
| Glycopyrrolate | 0.2–0.4 mg IV, IM | Antisialogogue | N/A |
| Dexmedetomidine |
Loading dose: 1 mcg/kg/min over 10 min |
Sedative | N/A |
| Midazolam | 0.5–4 mg IV | Sedative | Flumazenil |
| Fentanyl | 10–100 mcg IV | Opioid | Naloxone |
| Alfentanil | 100–1000 mcg IV | Opioid | Naloxone |
Topical Anesthesia of the Nose, Mouth, Tongue, & Pharynx
Figure 3: Topicalization of the mouth mucosa using a benzocaine spray.One way to achieve anesthesia for oral or nasal fiberoptic intubation is to topicalize the structures involved with a local anesthetic. Topicalization of the airway is the spreading of local anesthetic over a region of mucosa to achieve local uptake and neural blockade of that region.
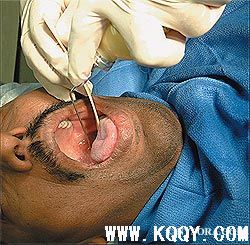
By far, the simplest of these techniques involves the spraying or swishing of local anesthetic directly onto themucosa of the mouth, pharynx, tongue, and/or nose. This can be accomplished with any of the many commercially available local anesthetics, particularly viscous lidocaine preparations and mixtures of benzocaine and tetracaine. The popular benzocaine (Cetacaine), a pressurized solution of benzocaine, tetracaine, and butamben in a small canister, delivers a spray via a long spray nozzle that is pointed in the desired direction (Figure 3). The anesthetic is delivered in an oily foam, which is absorbed rapidly into the mucosa and provides excellent topical anesthesia of the mucosa.
Alternatively, a 10-mL syringe can be filled with lidocaine 2–4% and sprayed via a small-bore single or multiperforated catheter or the working channel of the fiberoptic bronchoscope.11 This arrangement produces a fine stream of local anesthetic liquid, whichwith sufficient aliquots directed at the target mucosa achieves an adequate topical anesthetic effect. The safety and efficacy of both techniques are well established. Even with large amounts of swallowed anesthetic, plasma levels of local anesthetic should not reach toxic levels.12,13
Topicalization by Use of Local Anesthetic Reservoirs
Topicalization can also be accomplished by the use of local anesthetic-soaked cotton pledgets or swabs. These are soaked in either viscous or aqueous solutions of local anesthetic and then left for 5–15 minutes on the region of mucosa that requires anesthesia. The cotton acts as a reservoir for the anesthetic agent, producing a dense block. This technique is especially effective in the nasal passages. In the past, cocaine-soaked pledgets were used because they resulted both in a superb local anesthetic effect and in localized vasoconstriction. This practice has fallen out of favor, however, as concerns about cocaine toxicity grew. In addition, because of cocaine’s high profile as an illicit drug, there are significant regulatory hurdles associated with stocking it in a hospital formulary (eg, DEA paperwork, theft, accurate accounting of usage). As a method of achieving similar results, most clinicians have used the technique of adding small concentrations of epinephrine (1:200,000 or less) or phenylephrine (0.05%) to lidocaine. Alternatively, a vasoconstricting nasal spray can be applied before application of the local anesthetic. This approach results in dry mucosa, which then can be more easily anesthetized with local anesthetic because the local anesthetic does not get diluted with nasal secretions or saliva. The resulting vasoconstriction is nearly as effective as that of cocaine and offsets lidocaine’s powerful vasodilatation.
The applicationof highly concentrated local anesthetic-soaked cotton pledget reservoirs can be exploited to achieve highly specific nerve blocks as well. These methods are detailed later with the description of individual nerve blocks.
Inhalation of Aerosolized (Atomized) Local Anesthetic
Figure 4: Anesthetizing airway using inhalation of aerosolized lidocaine.Inhalation of aerosolized local anesthetic is another simple technique to achieve oropharyngeal anesthesia. To perform this technique, local anesthetic is added to a standard nebulizer with a mouthpiece or face mask attached. The patient is then asked to inhale the local anesthetic vapor deeply. After a period of approximately 15–30 minutes, the patient should have inhaled a sufficient quantity of local anesthetic to achieve a reasonably good level of topical anesthesia throughout the oropharynx and trachea. Focused aerosolized local anesthetic from an atomizer is ideal for nasal intubation. A number of disposable commercially available syringe-powered atomizers are available but are deficient in achieving small particle size unless outfitted with a side-stream air/oxygen flow to enhance dispersion by virtue of the Venturi principle (Figure 4).
For these techniques, lidocaine in concentrations of 0.5%–4% has been suggested; however, quicker and denser blockade is achieved by using concentrations in the range of 2–4%. This technique has a proven clinical track record of safety; however, little data are available regarding the blood levels of local anesthetic that are achieved using these techniques or regarding metabolism of swallowed local anesthetics. Parkes et al.[14] showed plasma concentrations of 0.29–0.45 mg/L in healthy volunteers after inhalation of 10% lidocaine solution. Because these levels were well below the generally accepted 5 mg/L safe level, it can be inferred that inhaling a 2–4% lidocaine for 15–30 minutes should be safe in most patients, particularly as a stand-alone technique.14
The major advantage of this technique lies in its simplicity and lack of discomfort. In addition, very little working knowledge of the anatomy of the region is required for its successful implementation.
Although this technique may seem ideal, it does have some drawbacks that limit its usefulness. The main disadvantage is that the density of the anesthesia achieved throughout the airway is highly variable. Many patients still experience an intact cough reflex, which can make intubation technically challenging. The rate of onset of this technique is highly dependent on patient compliance. Many patients who need an awake intubation are incapable or unwilling to take deep breaths. Also, inhalation of local anesthetic vapors can lead to central nervous system depression in patients whose mental status may already be depressed owing to other disease processes.
| Clinical Pearls | |
|
|
Techniques for Block Individual Nerves of the Airway
Blockade of the Glossopharyngeal Nerve
The oropharynx, soft palate, posterior portion of the tongue, and the pharyngeal surface of the epiglottis are innervated by the glossopharyngeal nerve. Block of the glossopharyngeal nerve facilitates endotracheal intubation by blocking the gag reflex associated with direct laryngoscopy as well as facilitating passage of a nasotracheal tube through the posterior pharynx. The glossopharyngeal nerve travels anterior along the lateral surface of the pharynx, and its three branches provide sensory innervation to the posterior third of the tongue, the vallecula, the anterior surface of the epiglottis (lingual branch), the walls of the pharynx (pharyngeal branch), and the tonsils (tonsillar branch). Logically, blockade of this nerve bilaterallywould result in anesthesia of those structures.
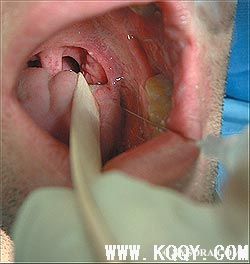
The glossopharyngeal nerve can be anesthetized using either intraoral or extraoral (peristyloid) approaches. For the intraoral approach, the mouth is opened and the tongue is anesthetized with topical anesthetic. A 3 1/3 -in., 22-gaugue needle is used to place 5 mL of local anesthetic solution submucosally at the caudal aspect of the posterior tonsillar pillar (palatopharyngeal fold) (Figure 5) To perform the peristyloid approach to the glossopharyngeal block, the patient is placed supine and a line is drawn between the angle of the mandible and the mastoid process. Using deep pressure, the styloid process is palpated just posterior to the angle of the jaw along this line, and a short, small-gauge needle is seated against the styloid process. The needle is then withdrawn slightly and directed posteriorly off the styloid process. As soon as bony contact is lost, 5–7 mL of local anesthetic solution are injected after careful aspiration for blood. Both approaches involve deposition of local anesthetic in close proximity to the carotid artery, and careful aspiration before injection is essential.
The applications of this block are limited by the specific anatomic regions that are innervated by the glossopharyngeal nerve. It is essential to ablate deep pressure symptoms from the tongue base during direct laryngoscopy. Blockade of the glossopharyngeal nerve is an integral part of effective block combinations, which is discussed later in the text.5 Because of the high vascularity of the palatoglossal arch, accidental vascular injection is an ever-present risk. Careful aspiration helps to reduce this risk, but it cannot be avoided entirely. In addition, significant absorption of local anesthetic can be expected in this region. The addition of epinephrine to the local anesthetic solution helps to vasoconstrict the blood vessels in the region, reducing absorption as well as assisting in the diagnosis of intravascular injection by heart rate monitoring. As with any injection into a highly vascular region, this techniquemay be contraindicated in patientswith coagulopathies or anticoagulation.
| Clinical Pearls | |
|
|
Superior Laryngeal Nerve Block
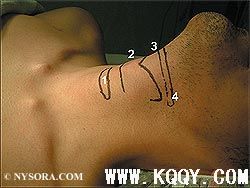
Figure 6: Surface anatomy of the larynx: (1) Cricoid cartilage; (2) thyroid cartilage; (3) hyoid bone; (4) cornu of the hyoid bone.The internal branch of the superior laryngeal nerve (a branch of the vagus nerve) provides sensory innervation to the base of the tongue, posterior surface of the epiglottis, aryepiglottic fold, and the arytenoids. Blockade of the sensory input to this branch can often be accomplished by mucosal saturation with local anesthetic by the inhalational and direct topical application techniques described above. In some patients, however, this may not provide timely adequate anesthesia for a comfortable awake intubation. In these cases, a direct regional blockade of the superior laryngeal nerve is desired. Regional anesthesia of the superior laryngeal nerve can be accomplished by exploiting the anatomic course of the nerve as it arises from the vagus nerve and descends to the larynx. The internal branch originates from the superior laryngeal nerve lateral to the greater cornu of the hyoid bone. In most patients, the nerve should pass approximately 2–4 mm inferior to the greater cornu of the hyoid bone.15 From here, it pierces the thyrohyoid membrane and travels under the mucosa in the pyriform recess.16
After topicalization, the most popular technique for superior laryngeal nerve block involves bilateral injections at the level of the greater cornu of the hyoid bone. The patient is placed supine with the head extended as much as possible. The patient’s skin is cleaned with an appropriate antimicrobial solution (eg, betadine). The cornu of the hyoid bone is located below the angle of the mandible. It is easily identified (particularly in men) by palpating outward from the thyroid notch along the upper border of the thyroid cartilage until the greater cornu is encountered just superior to its posterolateral margin (Figure 6). The nondominant hand is used to displace the hyoid bone with contralateral pressure, bringing the ipsilateral cornu and the internal branch of the superior laryngeal nerve toward the anesthesiologist. The anesthesiologist can then appreciate the pulsation of the carotid artery being displaced deep to the palpating finger tip.
A 5/8 -in., 25-gauge needle is inserted in an anteroinferomedial direction until the lateral aspect of the greater cornu is contacted (Figure 7). If the needle is then walked downward toward the midline (1–2 mm) off the inferior border of the greater cornu, the thyrohyoid membrane is pierced and the internal branch alone is blocked. If the needle is retracted slightly after contacting the hyoid, both the internal and external branches of the superior laryngeal nerve are blocked. The syringe is then aspirated, and if aspiration is negative for air and blood, 2 mL of local anesthetic (2% lidocaine) with or without epinephrine (1:300,000) are then injected. If aspiration results in air, the needle tip is likely in the larynx and needs to be retracted. If blood is encountered, the needle may have encountered a blood vessel. Given the proximity of the carotid artery, it is advisable to withdraw the needle, reassess the landmarks, and reattempt the procedure.
Two milliliters of local anesthetic should reliably bathe the internal branch of the superior laryngeal nerve, given its proximity to the hyoid bone. If this volume is injected outside the thyrohyoidmembrane, it is likely to block the external branch of the superior laryngeal nerve as well. Isolated external superior laryngeal nerve branch blockade may result in cricothyroid muscle weakness, which eliminates its function as an airway dilator.17 The motor input of the recurrent laryngeal nerve is spared, however, and therefore does not result in clinically significant change in laryngeal inlet diameters.18
The superior laryngeal nerve can also be approached in the pre-epiglottic space. The pre-epiglottic space is accessed at a point 2 cm lateral to the thyroid notch. The needle is advanced 1–1.5 cm superoposteriorly to pierce the thyrohyoid membrane, and the nerve can be injected. Alternatively, using the thyroid cornu as a landmark and walking the needle superoanteromedially can accomplish this block.
Some patients may be unwilling or unable to undergo such injections. Common reasons include patient refusal, anticoagulation, and distorted anatomy due to tumors, arteriovenous malformations, surgical deformities, or reconstruction. In patients in whom injection is contraindicated or overly challenging, a less invasive technique for blocking the superior laryngeal nerve can be accomplished by using soaked pledgets. After topicalization, the patient is asked to stick the tongue out. The tongue is then grasped using a gauze pad.With a right-angled forceps (Jackson-Krause forceps) the anesthetic-soaked pledgets are placed in the pyriform fossae located on either side of the root of the tongue. After 5–10 minutes, a sufficient degree of anesthesia should be present for intubation.19
| Clinical Pearls | |
|
|
Recurrent Laryngeal Nerve Block
The recurrent laryngeal nerve provides sensory innervation to the vocal folds and the trachea. Blockade of this nerve is necessary to provide comfort and prevent coughing while the endotracheal tube is being paused between the vocal cords. Sufficient blockade of the recurrent laryngeal nerve can often be accomplished using the inhalational technique previously described. Again, some patients may not achieve a sufficient amount of anesthesia to facilitate intubation.
Another technique for blocking the sensory input of the recurrent laryngeal nerve is the transtracheal block. In this technique, the cricothyroid membrane is located in the midline of the neck. It can be located by palpating the thyroid prominence and proceeding in a caudad direction. The cricothyroid membrane is identified as the spongy fibromuscular band between the thyroid and cricoid cartilages (Figure 8). After sterile skin preparation, the overlying skin is anesthetized by raising a small skin wheal of local anesthetic. Then a 22- or 20-gauge needle on a 10-mL syringewith 4mL of 4%lidocaine is passed perpendicular to the axis of the trachea and pierces the membrane. (Alternatively, a 20-gauge angiocath can be passed.)While the needle is being advanced, the syringe is continuously aspirated. The needle is advanced until air is freely aspirated, signifying that the needle is now in the larynx (Figure 9). Instillation of local anesthetic at this point invariably results in coughing. Through coughing, the local anesthetic is dispersed, diffusely blocking the sensory nerve endings of the recurrent laryngeal nerve. Motor function remains completely unaffected. It is advisable to use a larger-gauge needle for this block. A more rapid delivery of local anesthetic reduces the risk of needle-induced trauma due to coughing.
Direct blockade of the recurrent laryngeal nerve is contraindicated. This is because it may result in the upper airway obstruction, since the recurrent laryngeal nerve provides motor innervation for all themuscles of the larynx except the cricothyroid. In contrast, unilateral blockade typically manifests only as transient hoarseness.
| Clinical Pearls | |
|
|
Blockade of the Palatine Nerves
To allowawake nasal fiberoptic intubation, onemust also provide sensory blockade to the nasal passages. The greater and lesser palatine nerves innervate the nasal turbinates and the posterior two thirds of the nasal septum. The sensory input of these nerves can be blocked by topical application of the local anesthetic into nasal passages. If this proves inadequate, however, regional blockade of the palatine nerves can be accomplished by blocking the pterygopalatine ganglion from which both nerves arise. This can be accomplished noninvasively by taking a cotton-tipped applicator soaked in local anesthetic and passing it along the upper border of the middle turbinate to the posterior wall of the nasopharnx, where it is left for 5–10 minutes.20
An oral approach to the pterygopalatine ganglion is described with needle passage through the greater palatine foramen into the pterygopalatine fossa. A percutaneous approach via the mandibular notch is usual performed under fluoroscopic guidance for pain management. Because of technical difficulty and the high risk for vascular injury, these techniques are rarely needed or used for nasal-passage anesthesia during fiberoptic intubation. They are mentioned here only for the sake of completeness and academic discussion.
| Clinical Pearls | |
|
|
Blockade of the Anterior Ethmoid Nerve
The remaining portions of the nasal passages to be blocked are innervated by the anterior ethmoid nerve and is usually adequately blocked by inhalational or spray topicalization. This nerve can be selectively blocked by direct mucosal contact application with an anesthetic-soaked cotton applicator passed along the dorsal surface of the nose until the anterior cribiform plate is reached. The applicator is left in this position for 5–10 minutes.
| Clinical Pearls | |
|
|
Step-by-Step Method for Orotracheal Fiberoptic Intubation Using Topical Anesthesia Only
- Administer antisialogogue (glycopyrrolate 0.2–0.4 mg + dyphenhydramine (Benadryl) 20 mg IM) at least 20–30 minutes before fiberoptic instrumentation.
- Provide judicious sedation using appropriate doses of midazolam and fentanyl/alfentanil and/or dexmedetomidine.
- Use benzocaine spray to anesthetize the oral cavity and pharynx.
- Apply a generous amount of2%lidocaine ointment on the Ovassapian airway, and insert the tip of the airway in the patient’s mouth. As the lidocaine ointment is dissolved, it is carried deeper into the pharynx and swallowed by the patient. The airway is then advanced deeper as tolerated by the patient every 2–3 minutes. Eventually, the patient should be able to swallow the entire airway without discomfort.
- Attach a 5-mL syringe containing a solution of 4% lidocaine to the insufflating port of the flexible bronchoscope.
-
Advance the bronchoscope until the epiglottis and vocal chords are seen and proceed as follows:
- Inject 2 mL of local anesthetic over the epiglottis, wait 15 seconds, and advance the scope (anesthetizes the epiglottis and superior aspect of the cords).
- Inject 1mL of local anestheticwhen the tip of the scope is just above the vocal cords; wait 15 seconds and advance the scope (anesthetizes cords).
- Inject 2 mL of local anesthetic when the tip of the scope passes underneath the vocal cords (anesthetizes the trachea).
- Advance the scope until the carina is seen.
- Advance the endotracheal tube over the fiberoptic scope.
- If unable to intubate using the above method, attempt appropriate blockade of individual nerves until the patient is able to tolerate intubation.
Summary
An awake intubation often requires a combination of techniques to adequately anesthetize all the structures that will be encountered. The widest coverage is provided by the inhalational technique. This technique, however, does not always provide a dense enough level of anesthesia for all patients. Supplementation of this technique with any of the nerve specific blocks in this chapter is an excellent way to accomplish efficacious anesthesia for awake inubation.21
References
- Faccenda KA, Finucane BT: Complications of regional anaesthesia: Incidence and prevention. Drug Saf 2001;24:413–442.
- Auroy Y, Narchi P, Messiah A, et al: Serious complications related to regional anesthesia: Results of a prospective survey in France. Anesthesiology 1997;87:479–486.
- Naguib M,Magboul MM, Samarkandi AH, AttiaM: Adverse effects and drug interactions associated with local and regional anaesthesia. Drug Saf 1998;18:221–250.
- Cotter JT,Nielsen KC, GullerU, et al: Increased body mass index and ASA physical status IV are risk factors for block failure in ambulatory surgery: An analysis of 9,342 blocks. Can J Anaesth 2004;51:810– 816.
- American Society of Anesthesiologists Task Force on Management of the Difficult Airway: Practice guidelines for management of the difficult airway: An updated report by the American Society of Anesthesiologists Task Force on management of the difficult airway.Anesthesiology 2003; 98:1269–1277.
- Rose DK, Cohen MM: The airway: Problems and predictions in 18,500 patients. Can J Anaesth 1994;41:372–383.
- Netter F: Atlas of Human Anatomy. Ciba-Geigy Corporation, 1989, Plates 37–40.
- Netter F: Atlas of Human Anatomy. Ciba-Geigy Corporation, 1989, Plate 56.
- Avitsian R, Lin J, LottoM, Ebrahim Z: Dexmedetomidine and awake fiberoptic intubation for possible cervical spine myelopathy: A clinical series. J Neurosurg Anesthesiol 2005;17:97–99.
- Brookman CA, Teh HP, Morrison LM: Anticholinergics improve fibreoptic intubating conditions during general anaesthesia. Can J Anaesth 1997;44:165–regional_topical_anesthesia_for_endotracheal_intubation.
- Vloka JD, Hadzic A, Kitain E: A simple adaptation to the Olympus LF1 and LF2 fiberoptic bronchoscopes for instillation of local anesthetic. Anesthesiology 1995;82:792.
- Greenblatt DJ, BenjaminDM,Willis CR, et al: Lidocaine plasma concentrations following administration of intraoral lidocaine solution. Arch Otolaryngol 1985;111:298–300.
- Nydahl PA, Axelsson K: Venous blood concentration of lidocaine after nasopharyngeal applicationof 2%lidocaine gel.ActaAnaesthesiol Scand 1988;32:135–139.
- Parkes SB, Butler CS, Muller R: Plasma lignocaine concentration following nebulization for awake intubation. Anaesth Intensive Care 1997;25:369–371.
- Furlan JC: Anatomical study applied to anesthetic block technique of the superior laryngeal nerve. Acta Anaesthesiol Scand 2002;46:199– 202.
- Netter F: Atlas of Human Anatomy. Ciba-Geigy Corporation, 1989, Plates 70, 71.
- Wheatley JR, Brancatisano A, Engel LA: Respiratory-related activity of cricothyroid muscle in awake normal humans. J Appl Physiol 1991;70:2226–2232.
- .Woodson GE, Sant’Ambrogio F, Mathew O, Sant’Ambrogio G: Effects of cricothyroid muscle contraction on laryngeal resistance and glottic area. Ann Otol Rhinol Laryngol 1989;98:119–124.
- Curran J, Hamilton C, Taylor T: Topical analgesia before tracheal intubation. Anaesthesia 1975;30:765–768.
- Kundra P, Kutralam S, Ravishankar M: Local anaesthesia for awake fibreoptic nasotracheal intubation. Acta Anaesthesiol Scand 2000;44:511.
- Reasoner DK, Warner DS, Todd MM, et al: A comparison of anesthetic techniques for awake intubation in neurosurgical patients. J Neurosurg Anesthesiol 1995;7:94–99.
Next: Case Presentation: Cervical-Facial Cystic Hygroma
- Long Island College Hospital - [education]
- Faculty of Dental Medicine - H [education]
- The American Association of Or [organize]
- Summer Institute in Clinical D [organize]
- Academy of Osseointegration [organize]
- University of North Carolina a [education]
- American Orthodontic Society [article]
- American Equilibration Society [article]
- Niigata University - Japan [education]
- University of Buffalo [education]